Wisdom Teeth Extraction and Jaw Surgeries
Wisdom teeth, or third molars, are the last permanent teeth to appear (erupt) in the mouth. These teeth usually appear between the ages of 17 and 25. Some people never develop wisdom teeth. For others, wisdom teeth erupt normally — just as their other molars did — and cause no problems.
Many people develop impacted wisdom teeth — teeth that don’t have enough room to erupt into the mouth or develop normally. Impacted wisdom teeth may erupt only partially or not at all.
An impacted wisdom tooth may be:
Mesioangular: Grow at an angle toward the next tooth (second molar)
Distoangular: Grow at an angle toward the back of the mouth
Horizontal: Grow at a right angle to the other teeth, as if the wisdom tooth is “lying down” within the jawbone
Vertical: Grow straight up or down like other teeth but stay trapped within the jawbone
What Problems can occur with impacted wisdom teeth?
- Pain
- Trapping food and debris behind the wisdom tooth
- Infection or gum disease (periodontal disease)
- Tooth decay in a partially erupted wisdom tooth
- Damage to a nearby tooth or surrounding bone
- Development of a fluid-filled sac (cyst) around the wisdom tooth
- Complications with orthodontic treatments to straighten other teeth
Will wisdom teeth cause future dental problems?
It’s difficult to predict future problems with impacted wisdom teeth. However, If there isn’t enough space for the tooth to erupt, it’s often hard to get to it and clean it properly. Resulting food lodgement can give rise to tooth decay, gum problems and inflammation of the overlying gum.Older adults may experience difficulty with surgery and complications after surgery.
What you can expect
During the procedure
Your dentist or oral surgeon may use one of three types of anesthesia, depending on the expected complexity of the wisdom tooth extraction and your comfort level. Options include:
- Local anesthesia. Your dentist or oral surgeon administers local anesthesia with one or more injections near the site of each extraction. Before you receive an injection, your dentist or surgeon will likely apply a substance to your gums to numb them. You’re awake during the tooth extraction. Although you’ll feel some pressure and movement, you shouldn’t experience pain.
- Sedation anesthesia. Your dentist or oral surgeon gives you sedation anesthesia through an intravenous (IV) line in your arm. Sedation anesthesia suppresses your consciousness during the procedure. You don’t feel any pain and will have limited memory of the procedure. You’ll also receive local anesthesia to numb your gums.
- General anesthesia. In special situations, you may be offered general anesthesia. You may inhale medication through your nose or have an IV line in your arm, or both. Then you lose consciousness. Your surgical team closely monitors your medication, breathing, temperature, fluids and blood pressure. You’ll experience no pain and have no memory of the procedure. Local anesthesia is also given to help with postoperative discomfort.
During wisdom tooth extraction, your dentist or oral surgeon:
- Makes an incision in the gum tissue to expose the tooth and bone
- Removes bone that blocks access to the tooth root
- Divides the tooth into sections if it’s easier to remove in pieces
- Removes the tooth
- Cleans the site of the removed tooth of any debris from the tooth or bone
- Stitches the wound closed to promote healing, though this isn’t always necessary
- Places gauze over the extraction site to control bleeding and to help a blood clot form
After the procedure
If you receive sedation anesthesia or general anesthesia, you’re taken to a recovery room after the procedure. If you have local anesthesia, your brief recovery time is likely in the dental chair.
As you heal from your surgery, follow your dentist’s instructions on:
- Bleeding. Some oozing of blood may occur the first day after wisdom tooth removal. Try to avoid excessive spitting so that you don’t dislodge the blood clot from the socket. Replace gauze over the extraction site as directed by your dentist or oral surgeon.
- Pain management. You may be able to manage pain with an over-the-counter pain reliever, such as acetaminophen (Tylenol, others), or a prescription pain medication from your dentist or oral surgeon. Prescription pain medication may be especially helpful if bone has been removed during the procedure. Holding a cold pack against your jaw also may relieve pain.
- Swelling and bruising. Use an ice pack as directed by your dentist or surgeon. Any swelling of your cheeks usually improves in two or three days. Bruising may take several more days to resolve.
- Activity. After your surgery, plan to rest for the remainder of the day. Resume normal activities the next day, but for at least a week, avoid strenuous activity that might result in losing the blood clot from the socket.
- Beverages. Drink lots of water after the surgery. Don’t drink alcoholic, caffeinated, carbonated or hot beverages in the first 24 hours. Don’t drink with a straw for at least a week because the sucking action can dislodge the blood clot from the socket.
- Food. Eat only soft foods for the first 24 hours. Start eating semisoft foods when you can tolerate them. Avoid hard, chewy, hot or spicy foods that might get stuck in the socket or irritate the wound.
- Cleaning your mouth. Don’t brush your teeth, rinse your mouth, spit or use mouthwash during the first 24 hours after surgery. Typically you’ll be told to resume brushing your teeth after the first 24 hours. Be particularly gentle near the surgical wound when brushing and gently rinse your mouth with warm salt water every two hours and after meals for a week.
- Tobacco and alcohol use. If you smoke, don’t do so for at least 72 hours after surgery — and wait longer than that if possible. If you chew tobacco, don’t use it for at least a week. Using tobacco products and alcohol after oral surgery can delay healing and increase the risk of complications.
- Stitches. You may have stitches that dissolve within a few weeks or no stitches at all. If your stitches need to be removed, schedule an appointment to have them taken out.
Risks
Most wisdom tooth extractions don’t result in long-term complications. However, removal of impacted wisdom teeth occasionally requires a surgical approach that involves making an incision in the gum tissue and removing bone. Rarely, complications can include:
- Painful dry socket, or exposure of bone when the post-surgical blood clot is lost from the site of the surgical wound (socket)
- Infection in the socket from bacteria or trapped food particles
- Damage to nearby teeth, nerves, jawbone or sinus
In addition to making the area numb with local anaesthetic, your surgeon may suggest sedation to allow you to be more comfortable during the procedure. A wisdom tooth extraction is almost always performed as an outpatient procedure. This means that you go home the same day.
You’ll receive instructions from the hospital or dental clinic staff on what to do before the surgery and the day of your scheduled surgery.
When to call your dentist or surgeon
Call your dentist or oral surgeon if you experience any of the following signs or symptoms, which could indicate an infection, nerve damage or other serious complication:
- Difficulty swallowing or breathing
- Excessive bleeding
- Fever
- Severe pain not relieved by prescribed pain medications
- Swelling that worsens after two or three days
- A bad taste in your mouth not removed with saltwater rinsing
- Pus in or oozing from the socket
- Persistent numbness or loss of feeling
- Blood or pus in nasal discharge
Follow up appointments:
You probably won’t need a follow-up appointment after a wisdom tooth extraction if:
- You don’t need stitches removed
- No complications arose during the procedure
- You don’t experience persistent problems, such as pain, swelling, numbness or bleeding — complications that might indicate infection, nerve damage or other problems.


Jaw surgery
Orthognathic surgery, or simply jaw surgery, is surgery designed to correct conditions of the jaw and lower face related to structure, growth, airway issues including sleep apnea, TMJ disorders, alignment problems primarily arising from skeletal disharmonies, dental bite problems that cannot be easily treated with braces alone.
Difficulty in the following areas should be evaluated for the possible need for corrective jaw surgery:
- Difficulty in Chewing, Biting or Swallowing
- Speech Problems
- Chronic Jaw or TMJ Pain
- Open Bite (teeth don’t touch together)
- Protruding Jaw
- Breathing Problems
- Underbite
- Overbite
- Small Chin/Retruded Jaw
- Obstructive Sleep Apnea
- Snoring
- Jaw, chin, and nose misaligned
Who performs these surgeries?
Jaw surgery is performed by maxillofacial or an oral surgeon or a plastic surgeon in collaboration with an orthodontist. It often includes braces before and after surgery, and retainers after the final removal of braces. Orthognathic surgery is often needed after reconstruction of cleft palate or other major craniofacial anomalies. Careful coordination between the surgeon and orthodontist is essential to ensure that the teeth will fit correctly after the surgery.
How is this surgery planned?
Planning for the surgery usually involves input from a multidisciplinary team, including oral and maxillofacial surgeons, orthodontists, and occasionally a speech and language therapist. Although it depends on the reason for surgery, working with a speech and language therapist in advance can help minimize potential relapse. The surgery usually results in a noticeable change in the patient’s face; a psychological assessment is occasionally required to assess patient’s need for surgery and its predicted effect on the patient. CT scans, xrays and photographs are taken to help in the planning. A virtual surgery software helps to predict the shape of the patients face post-surgery. Great care needs to be taken during the planning phase to maximize airway patency.
Why are braces required for this surgery?
Orthodontics are a critical component of orthognathic surgery. Traditionally the presurgical orthodontic phase can take as long as one year and undertaken with conventional metal braces. However, these days new approaches and paradigms exist including surgery-first and using clear aligner orthodontia (like Invisalign).
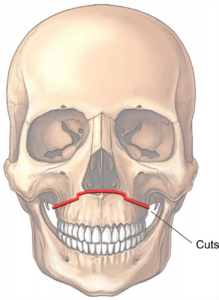
What is upper jaw surgery/ Le Fort 1 osteotomy?
The LeFort I osteotomy is commonly used for the correction of severe overbites,underbites and jaw deformities as it allows movement in all 3 planes. Furthermore, it is commonly used to treat midface hypoplasia and gummy smiles. An underbite associated with maxillary hypoplasia is commonly found in patients with orofacial clefts, obstructive sleep apnea (OSA), and maxillary atrophy. Combined with lower jaw surgery, it improves the esthetics for patients with facial asymmetry .
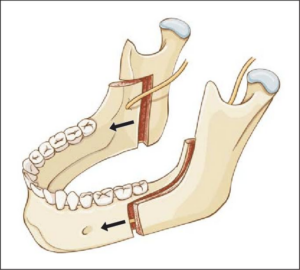
What is lower jaw surgery?
The bilateral sagittal split osteotomy(BSSO) is probably one of the most versatile surgical procedures performed for advancing or retruding the lower jaw. A BSSO can be performed alone or in combination with an upper jaw or chin surgery. Braces continue for several months before and after the surgery.
The operation is almost entirely carried out from the inside of the mouth to minimise visible scars on the skin of the face. A cut is made through the gum behind the back teeth to gain access to the jawbone. The lower jaw is then cut with a small saw to allow it to be broken in a controlled manner. It is then moved into its new position and held in place with small metal plates and screws.
Occasionally it is necessary to make a small “stab” incision on the skin of the face to allow the screws to be inserted. This incision is a few millimetres long and usually only requires a single stitch to hold it back together. The gum inside the mouth is stitched back into place with dissolvable stitches that can take a fortnight or even longer to fall out.
What is chin surgery?
Genioplasty or Chin surgery, is a surgical procedure to reshape the chin either by enhancement with an implant or reduction surgery on the bone. Oral-maxillofacial surgeons with specific training and experience in treating the head, face, mouth, and jaw typically perform genioplasty procedures.
However, plastic surgeons can also perform this type of surgery if they have the necessary training and experience. People typically receive general anesthesia before a genioplasty procedure.
The exact operation and recovery times vary, depending on the type of genioplasty a person is undergoing and the extent of corrections a surgeon is performing.
Surgeons use chin repositioning surgery to correct the following problems:
- Receding chins, or retrogenia
- Overly large or extended chins
- Chins that are too short or too tall
- Misaligned or asymmetrical chins
- Abnormal dental bite
- Sleep apnea in combination with other skeletal surgeries
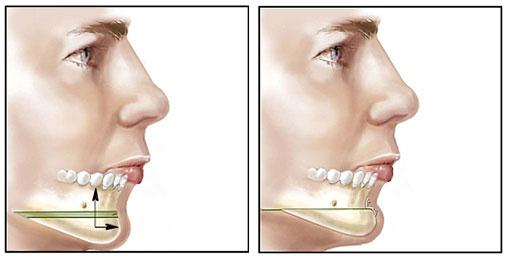
Virtual 3D Surgical Planning
The virtual surgical planning has been used for numerous types of jaw surgery procedures. First, obtaining an accurate and detailed representation of facial asymmetries is a valuable diagnostic tool. Second, the technique allows for adjustments in simulating different operative techniques, which translates into customized treatment plans and better outcomes.
PRE SURGERY
POST SURGERY SIMULATION