Pediatric Snoring and Sleep Apnea
Pediatric snoring
Snoring can be a clue that your child is not getting good quality sleep and when air cannot flow freely through the airway at the back of the throat. As a person inhales or exhales, tissue around the airway vibrates, creating an audible noise.
Multiple factors can create blockages of the airway and cause a person to snore. In children, the most common risk factors for snoring include:
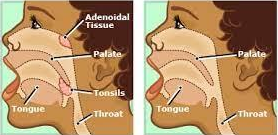
❖ Large/Swollen Tonsils and Adenoids: Tonsils and Adenoids are found near the back of the throat, and they are part of the body’s immune system. If they are naturally larger or are swollen because of infection, the tonsils and adenoids can obstruct the airway and cause snoring.
❖ Obesity: Studies have found that children who are overweight are more likely to snore. Obesity can narrow the airway and raise the risk for SDB including obstructive sleep apnea.
❖ Congestion: Cold-like symptoms can cause congestion that blocks the smooth flow of air, and infection may inflame the tonsils and adenoids.
❖ Allergies: Flare-ups of allergies can cause inflammation in the nose and throat that can make it harder to breathe and raise the risk of snoring.
❖ Asthma: Like allergies, asthma may inhibit normal breathing, and if it causes partial blockages of the airway, can provoke snoring.
❖ Anatomic characteristics: People have anatomic characteristics that make it harder for them to breathe normally when sleeping. For example, a deviated septum, in which the nostrils are not separated equally, may cause mouth-breathing and snoring.
❖ Environmental Tobacco Smoke (ETS): Exposure to ETS, often referred to as secondhand smoke, can affect breathing and has been correlated with a higher risk of snoring in children.
❖ Contaminated Air: Low air quality or excess contaminants can pose a challenge to normal respiration and may influence a child’s chances of frequent snoring.
❖ Shorter duration of Breast-feeding: Research has found an association between snoring in children and reduced duration
of breast-feeding. The exact reason for this is unknown, but it may be that breastfeeding helps the upper airway develop in a way that cuts down on the likelihood of snoring.
FAQ'S
When snoring becomes more frequent and interrupts sleep, it can indicate the presence of Sleep Disordered Breathing (SDB). Talk to your Pediatrician if you notice these red flags:
∙ Your child snores most nights of the week.
∙ You frequently hear snoring during the night.
∙ The snoring is very noisy.
∙ Your child routinely sleeps with his or her mouth open, and chin or neck extended.
∙ You hear your child pause or gasp while sleeping.
∙ Craniofacial disorders (often from birth defects like cleft palate or cleft lip, or from trauma).
∙ Certain genetic disorders (such as Down syndrome).
∙ Some neuromuscular disorders (such as cerebral palsy and muscular dystrophy).
∙ Sickle cell disease.
∙ Bedwetting
∙ Bluish skin
∙ Morning headaches
∙ Daytime sleepiness
∙ Difficulty concentrating or learning
∙ Diagnosis of attention-deficit/hyperactivity disorder (ADHD) ∙ Below-average weight gain
∙ Obesity
A Paediatrician, a Sleep Physician or an ENT surgeon.
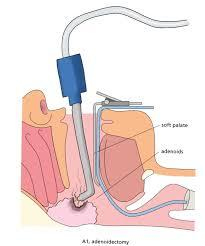
Adenoid & Tonsil Surgery:
If swollen adenoids and tonsils bother your child and dont respond to medicines, then a health care provider may recommend an Adenotonsillectomy.Surgery remains the mainstay of treatment.

Jaw expansion before the child is 12 years old opens up the nose and makes breathing easier. It also helps to create space to correct crooked teeth.